Business as usual in the high acuity core of the emergency department. Patients coming and going. The early morning hustle and bustle of nurses, techs, respiratory therapists, residents and attendings. The hum of monitors, the beeps of various alarms and the buzz of fingers feverishly typing at computer stations. Overhead, we hear the monotone hospital announcer’s voice through the intercom system: “CODE BLUE. First floor. Short-term cardiac care unit. Room…”
This announcement was followed by a brief pause throughout the entire emergency department core as those words sank in to everyone’s understanding. First floor, that’s us. Explosions of noise and motion followed the stillness of that moment as nearly everyone dropped what they were doing and began to sprint down the hall towards the short-term cardiac care unit. My senior resident tells me to grab the airway box. I do so and follow suit running down the hall.
Less than a minute later, everyone arrives at the small cardiac observation room where cardiopulmonary resuscitation (CPR) had already begun. We pass the patient’s loved one outside, held by a nurse while she cries silently and covers her mouth with a hand. She is shocked by not knowing what may happen.
Providers pour into the room. Jolts of movement pass through the patient’s body with each violent chest compression. A resident is beginning to work on accessing an airway. My senior resident quickly establishes herself as leader of the code, and all information and decisions pass through her. No pulse. No breathing. ABC: Airway, breathing, circulation.
My senior residents says, “Put the patient on the monitor and intubate.” Two minutes go by. “Give epi (epinephrine).” Still no pulse. “BACK ON THE CHEST.”
I rotated in to pick up where the last compressor left off, pushing on the center of the patient’s chest, trying to remember my American Heart Association basic life support (BLS) class — compressions are given at the rate of “Stayin’ Alive,” so I compress while mentally singing, “Ah, ah, ah, ah, stayin’ alive.” I compress two whole inches inward towards the patient’s center and allow for recoil. I feel the resistance of the patient’s chest increase as he laryngospasms with the passage of the breathing tube down his trachea. I think to myself, “Is this really happening?” I look to my senior resident for any commands and wait for the two-minute mark to allow another person to rotate in and allow me to rotate out of CPR.
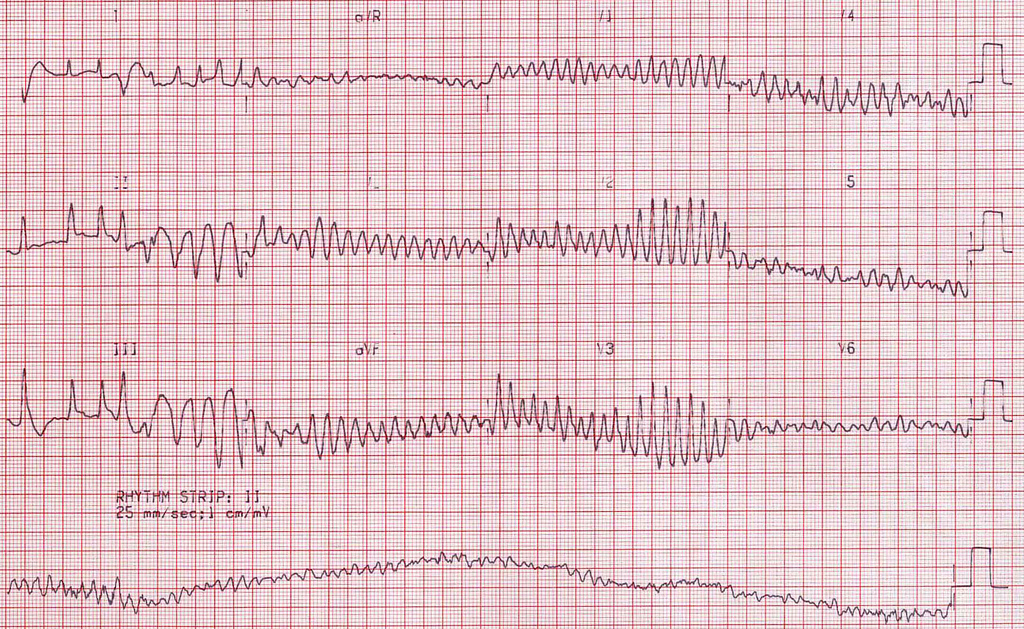
Our code leader speaks again, “Hold CPR! Another round of epi! He’s in v-fib (ventricular fibrillation). Prepare to shock! Back on the chest while the machine charges [to the determined voltage].” *machine charges as chest compressions continue* “Everybody clear?”
We all respond, “Clear!” The patient’s limp body jumps as the shock is delivered, and CPR continues immediately afterwards. My senior resident consults with the cardiologist in the room, and they decide what medications to proceed with as the advanced cardiac life support (ACLS) algorithm continues to unfold.
After fifteen minutes in cardiac arrest, with multiple shocks, multiple doses of epinephrine and amiodarone, an intubation and consistent CPR, the patient returned to a sinus rhythm which allowed him to deliver blood to his body without the help of our chest compressions. Color began to return to his blue face and extremities. My senior resident who lead the entire code dismissed many members of the resuscitation team who were no longer needed to protect the patient. She and several other providers stayed to ensure the patient was stabilized and transferred quickly to the cardiac catheterization lab and then the cardiac intensive care unit (ICU). And just like that, it was over. I returned to the emergency department to continue seeing patients.
—
What a mix of emotions. I felt the rush of adrenaline during the resuscitation. I felt exhilarated afterwards thinking, so this is what it feels like to help bring someone back to life. I felt the anxiety mixed with excitement as I delivered my first chest compressions to a real patient. And, after, everyone just seemed to go back to work as if nothing happened.
There was a strange tension in my mind that oscillated between the excitement, rush, exhilaration, and, frankly, enjoyment of participating in a code. His impending death in that moment, the impact of the experience on his loved one and the possibility that the code could just as easily end with a time of death pronouncement all played into my emotions. If the code had not gone as planned, I wondered what this patient’s life would look like now. Would he have made it to the end of the day? If he did, what sequelae of his arrest would he have? How would his brain function after being deprived of normal amounts of oxygen for so long? I can only hope that our medical interventions were successful and this patient has a little more precious time to spend with those who love him.
It was also a stark experience of the reality that in medicine the dynamics can change so dramatically from one moment to the next. For example, in a matter of minutes, I went from helping save a patient’s life during a code only to return to the emergency department and share a new diagnosis of cancer with another patient. What a unique profession where we have the opportunity to participate in such significant moments in people’s lives.
Even now, I do not know whether that patient ever made it out of the hospital alive. I hope he did. But, I am grateful for having had the experience. I am grateful for the chance to be a part of his care and a part of the team that responded to his cardiac arrest. It was an amazing experience, and I learned so much from this brief interaction. In the future, I will remember the experience and apply what I learned. I will attempt to remain composed and respond appropriately when I eventually find myself as the physician leading the code team and deciding how best to try and save a patient’s life.
Image credit: “MS” (CC BY-NC 2.0) by Popfossa