When examining my post-graduate career options, I look closely into the statistics regarding women in surgery in the countries I am interested in training in. It seems a fairly manipulative factor to consider when weighing post-graduate training options, but if the odds are against me because of something as irrelevant as my gender, then I would be unwise not to consider this and try to stack the deck, to some extent, in my favor.
An obvious option for an Irish medical student, like myself, looking to work in another health service is the National Health Service (NHS) in the United Kingdom. The NHS, though not without its faults, has often been recognized as a well-organized, high-functioning health service. The U.K. is also a comfortable option with its mild weather, English language, and short distance from home. On a recent trip to London, I heard the automated voice at tube stops warning me to “mind the gap,” and it occurred to me that perhaps the same recording should be played to female medical students upon graduation. There is a lot to be gained from going to the United Kingdom, but in reality, the gender gap between male and female surgical trainees is significant. A recent television documentary, “Confessions of a Junior Doctor,” revealed that a significant number of female surgical trainees drop out because of the pressure of the long hours and lack of family support. Exact statistics are not available, but a quick look at women in surgical training schemes compared to those in consultancy positions can give some light to this issue.
Only 11 percent of consultant surgeons in the United Kingdom in 2015 were female. This statistic is higher than in Ireland, as only seven percent of Irish surgical consultants are women. However, neither of these statistics is of any real comfort, especially when one considers that more than 50 percent of medical school graduates in Ireland are women.
A 2013 study carried out in the United Kingdom examined the opinions of recent medical graduates regarding surgery as a career option and, astonishingly, 68 percent of females indicated they felt surgery was not a welcoming career for women. These statistics throw up red flags for me while I consider post-graduate options. Though these numbers do not drive me as far as reconsidering surgery, these opinions urge me to reconsider a health service where the vast majority of recent female medical graduates feel unwelcome to participate in a major specialty of medicine.
The United States does not fare much better, statistically. Between 1970 and 2008, the number of surgeons in the United States increased by just seven percent. In 2008, there were 160,000 surgeons in the U.S. and only 19 percent of these were female. Though this is still not ideal, this is one of the more encouraging female-to-male ratios I came across. It should also be noted, and appreciated, that the number of women who are chairs of departments of surgery has risen significantly with 18 women across the U.S. holding the title of chair of surgery in 2015.
“Women in surgery” is commonly controversial, with many who believe the long hours and intense training programs are incompatible with having a family. I am under no illusions that it is easy, but I also have never heard of any male classmates asked, “what about kids?” when they say they are pursuing surgery. I have lost count of the number of times I have been asked a similar question. The issue is not the stressful training; the issue lies in the assumption that all child-rearing is the responsibility of the woman. I remember reading a biography of a female surgeon who, when asked how she would operate when pregnant, quipped that she would just stand a little further back from the table. The “issue” of pregnant women and mothers as surgeons has only become an issue because of the external influence of a society that believes a woman’s role is always as the primary care giver.
The Royal College of Surgeons in Ireland has recently launched an initiative to encourage more female graduates to consider surgery, a move that I find hopeful. Similarly, in 2007, the Royal College of Surgeons in the United Kingdom launched the Women in Surgery initiative to “encourage, enable and inspire” women to fulfill their ambitions for a career in surgery. Such initiatives are inspiring, but only time will tell how beneficial they will be in narrowing the gender gap in surgery.
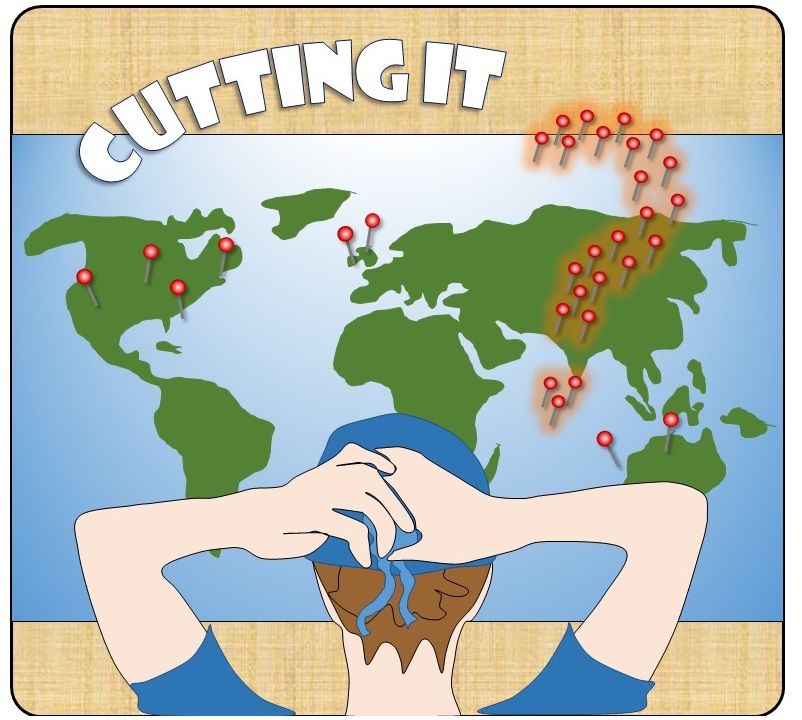
I have looked at the statistics and I have weighed the odds; the truth is, there is no “good” country to be a female surgeon. Given the nearly similar gender gaps across the board, its consideration does not add much benefit when weighing post-graduate career options. The gender gap certainly matters, but with every country I look at, regardless of where in the world it is, the concern for gender discrepancy is the same. The majority of medical school graduates are women, but the minority of surgeons and surgical trainees are women. The one thing that transcends all cultures appears to be a global sluggishness to welcome women into the surgical ranks. Though it is disappointing, this does not particularly deter me. Surgery is a difficult career, whatever way you cut it — no pun intended. There will always be issues to overcome, and being aware of them is half the battle. Onwards and upwards.
A medical degree offers students a global skill, where they can work anywhere in the world. But in reality, how easy it is to leave one health service for another? Join Suzanne as she navigates studying in Ireland while planning for a surgical residency abroad.