When Advocating Becomes Difficult: Health Care Professionals and War
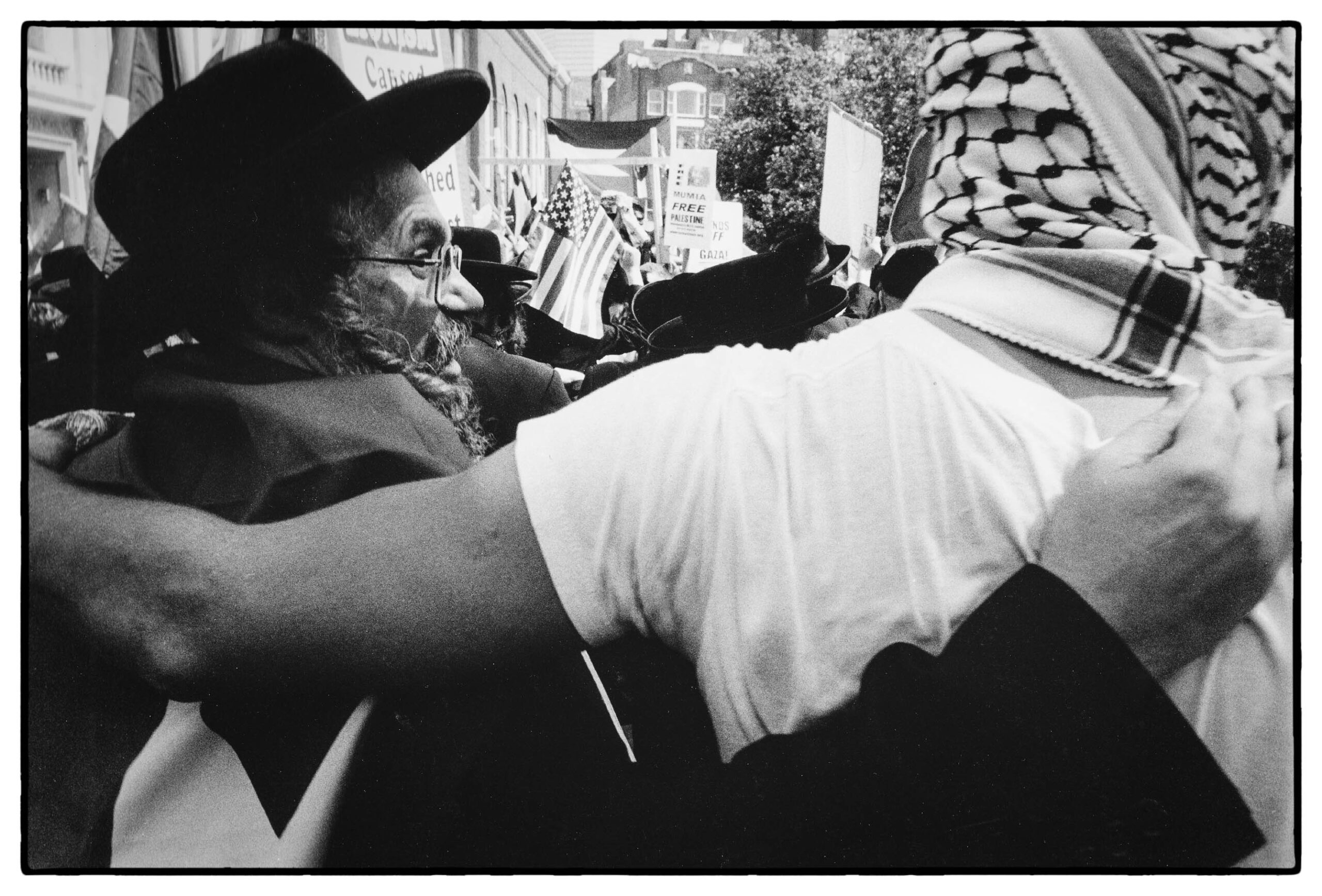
The purpose of this piece is not to assign blame, nor is it to debate the inciting event for the current state of the people in Gaza. Instead, I hope to inspire you, the reader, to set aside any political differences and to lean into your role as both a human and patient advocate. I urge you to speak up in support of our colleagues overseas, who are treating and operating under the threat of death; for history will not judge our silence kindly.