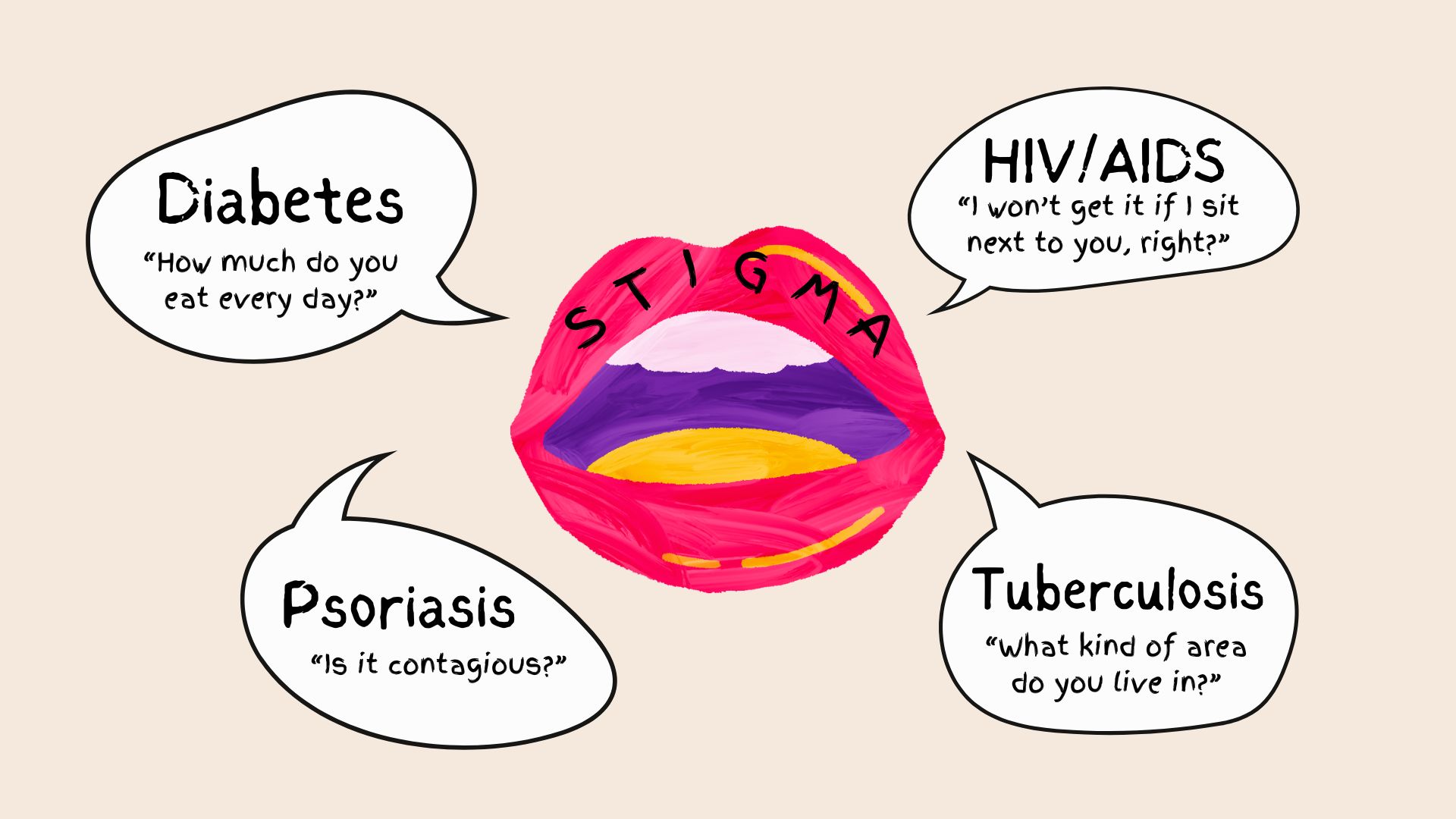
Complexity to Be Unfolded: from “Swiss Army Knife” to “Coexistence”
Science, in German, is Wissenschaft, which translates to “pursuit of knowledge” in English. I recently finished my neuroscience PhD training and revisited my scientific journey spanning from my teenage years to my PhD thesis. As a teenager, I was busy memorizing knowledge from textbooks. As an undergraduate, I had some experiences where I learned that science is not always as clear-cut as what I was taught in classes. As a PhD student, I have been trained to look at scientific findings with a critical eye and always ask if they are accurate.