Open sewage ran beside homes made of handmade brick in Pau da Lima. In a valley of the favela in Salvador, Brazil, my fieldwork team usually ate our lunches in the shade, conversing with an elderly man who operated a makeshift market. He sold goods to those who were unable or unwilling to scale the characteristically steep hills in order to enter the nearby city.
My path to this favela, like my journey in medicine, felt unconventional. This was the first memory that popped into my head when I was asked to reflect on the role of microbiology in my life as part of a final assignment in my microbiology block. I realized microbes may have coincidentally been the root of my decision to pursue a career in medicine.
I studied ecology and evolutionary biology as an undergraduate student. After enrolling in an introductory biology course, thinking I would major in philosophy, ecology rekindled and reminded me of my love for nature and the wonder of the great outdoors. I trained as a whitewater raft guide in high school and was on the varsity women’s crew team in college. Naturally, I drifted towards another avenue in which I could be on the water: freshwater ecology.
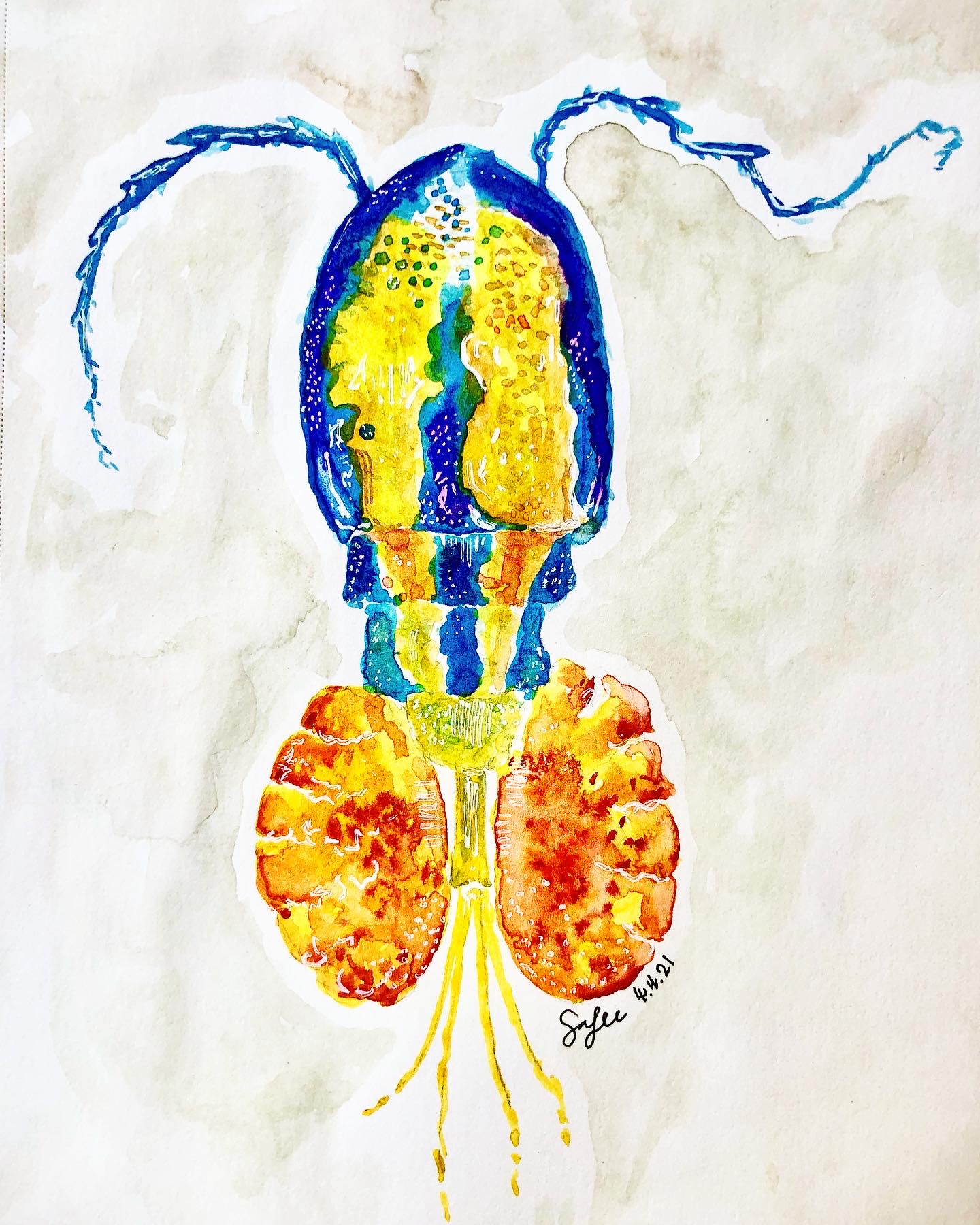
In my favorite campus job at Yale University, I was a laboratory assistant in a freshwater ecology lab. I spent most of my days collecting samples from nearby freshwater lakes in Connecticut and analyzing them to monitor water quality. It was idyllic and Walden-esque — I soaked up the sun on a beautiful day while drifting on a wooden boat, all in the name of science. Returning to the laboratory, I would peer through the microscope, seeing different microorganisms. These included copepods — which I would later learn could be vectors for Dracunculus species in my microbiology block as well as various species of Daphnia.
For my thesis, I ended up spending countless hours culturing my own little tank ecosystems filled with Daphnia — my cheap alternative to Sea Monkeys. I examined how different environmental stressors would lead to changes in their development. Through this work, I hoped to extrapolate how these stressors — heat, toxicity, food availability — might surface in different ecosystems to serve as proxies for environmental health.
None of this involved human health outcomes, unless you count my possible consumption of contaminated lake water (I am slightly convinced of my own invincibility now that I am aware of what organisms can thrive in polluted water.) However, the skills I gained from ecology — fieldwork, laboratory research, data analyses and writing — taught me to love scientific inquiry.
I put those tools to use in another lab when I saw another available campus job as a research assistant: this time, in the School of Public Health with vector-borne disease. I helped analyze patient cases and serologies of babesiosis, which is carried by the Ixodes tick, commonly seen in the American Northeast. On one occasion, I accompanied the principal investigator and his team to Block Island in Rhode Island. We collected blood samples from these patients. I learned during this block that these would exhibit characteristic “Maltese crosses” in thin blood smears.
This intersection of ecology and disease led me to the city of Salvador, Brazil after graduation. I wore a white laboratory coat to signal that I was a researcher with Fiocruz Bahia, a trusted national biomedical research organization. Everyday, I entered the neighborhood with a team of nurses to examine how rat population dynamics would affect leptospirosis transmission and variation in levels of pathogens in the water in the favela. Ironically, this coat led to unexpected consequences as people stopped me when I was collecting environmental samples from the open sewage and soil, mistaking me for a doctor.
At times, they would ask me medical questions that I likely still do not know the answer to. However, these conversations were numerous and provided intimate insight into the health care issues that plagued the region. Diagnoses were not sought until symptoms reared, and triaging at the local public emergency room often meant hours of waiting for treatment. It could come too little, too late or never.
Over the year I lived in Salvador, I began to realize that studying ecology and being outdoors was something that I loved doing. I yearned, however, for a more direct impact on human health outcomes. I realized a medical degree would lend skills needed to directly care for patients as well as conduct informed and impactful research. Coming back to the United States while finishing my pre-medical requirements, I continued to research infectious disease; however, I examined a decidedly more human aspect of it: the sociocultural determinants in seeking prophylactic and antiretroviral treatment for HIV.
I initially thought I would become an infectious disease doctor; it seemed only logical that the passions and skills that I had built until this point would set me down this path. It seems ironic that I would enter medical school in the middle of a global coronavirus pandemic, in a way further adding to my story of infectious disease guiding my life choices.
Regardless of whether I continue in microbiology, infectious disease or an entirely different course, I find joy in learning and researching areas of which I had little prior understanding. I could not have foreseen that microbial organisms would lead me to medicine, but look forward to the path that medicine leads me towards. Perhaps from force of habit, I imagine this journey to be not dissimilar to fieldwork.
Images courtesy of Yeonsoo Sara Lee.