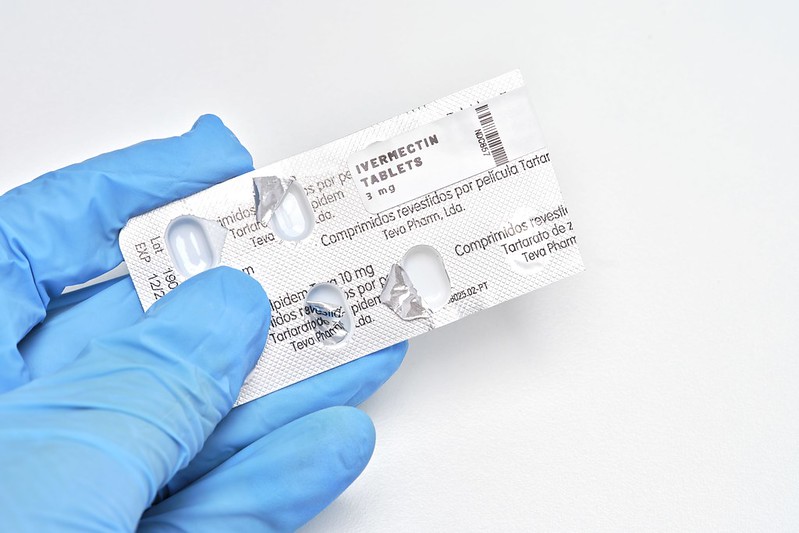
Like many medical students, I am familiar with the antiparasitic medication ivermectin, a common drug taught in medical school. Ivermectin became an unexpected subject in the COVID-19 pandemic. However, after seeing a patient in the clinic taking ivermectin as an alternative to vaccination, the news hit differently.
Along with many health care workers, I was frustrated given the already low vaccination rate. I was puzzled about how ivermectin, like hydroxychloroquine, became a subject of discourse in COVID-19 treatments. There was a lack of evidence regarding the efficacy of ivermectin on treating COVID-19. However, an assortment of advocacy groups and online communities continue to tout the drug as the solution to the pandemic, further frustrating public health officials to clarify the record and urge the public to not use it outside of clinical trials.
The surge of misinformation, what the World Health Organization calls an infodemic, has been an undeniable aspect of the pandemic. We live in the age where social media is increasingly becoming the primary form of obtaining information. Their algorithms, which seeks to keep users engaged on their platforms, compounded the ability for misinformation to spread. In response, social media companies have begun restricting and flagging posts pertaining to COVID-19.
But before COVID-19, there had been problems with health misinformation in the past. Tobacco companies employed tactics to diminish the reliability of studies that link smoking and lung cancer. As recent as 2006, a Harper’s Magazine essay stroked controversy for supporting AIDS denialism, a pseudoscientific position that refuses to acknowledge that HIV causes AIDS.
In the context of our information overloaded society, I believe a major reason for the prevalence of misinformation surrounding COVID-19 is its novelty. We are constantly bombarded with the ever-changing information streaming into our homes, our cars, and our phones. Information about COVID-19, particularly in the beginning of the pandemic, was evolving and changing, sometimes backtracking to initial impressions.
As a medical student, I am expected to practice evidence-based medicine, dissecting the evolving scientific literature and evaluating the strength of the evidence, methodology, and credibility of the latest publications. This is not to say that COVID-19 was neither disruptive nor that medical students had difficulties adapting to the COVID-19 environment. However, as medical students, we had the necessary tools to navigate the ever-changing landscape regarding our understanding of COVID-19.
For many in the general public, it can be overwhelming to digest what’s happening. I do not blame them. After all, there are many stressors in life. With COVID-19 amplifying them, people are already exerting their mental energy and financial resources. Additionally, people are not often taught how to evaluate information like the way they teach us to do so in medical school. This makes it a prime environment for misinformation to spread. Undoubtedly, it does not help when public figures are the ones spreading misinformation.
What’s more disturbing, however, is when people with credentials are the ones participating in the spread of misinformation. In the past year, these experts have asserted that COVID-19 was caused by 5G radio frequencies, advocated against the COVID-19 vaccines, and go as far as saying the pandemic is “the greatest hoax ever perpetuated.”
The Federation of State Medical Boards stated that medical licenses could be suspended or even revoked from physicians spreading misinformation about COVID. That statement was supported by the American Academic of Pediatrics, American College of Physicians, and American Academy of Family Physicians.
And there are reasons for such a strong reaction. Scientists and physicians occupy an extremely trusted position in society, and when those with the credentials abuse it, it can have terrifying consequences.
Looking back, I can better appreciate the patient’s perspectives as they were taking ivermectin. They probably had heard about it from someone they trust. Maybe they saw a video online of someone saying that they have the right credentials, they’re smart, and they know the “science.”
Now more than ever, it is important to be conscientious and intentional during interactions with patients, regardless of their level of understanding or the resources that they might use. And yes, that includes the conspiracy theories and the “quacky” solutions.
As a result, I was disappointed about how the Food and Drug Administration (FDA) posted about ivermectin without considering how patient understand the medication. By dismissing the people’s health concerns regarding treatments as ridiculous, it does not help to convince people to take the vaccination. It’s worth reminding that those that have advocated for alternatives to vaccinations already do not trust the FDA.
Even with a vaccine mandate, many people must still want to receive the COVID-19 vaccine. One of the best ways to encourage for people to take the vaccination is to provide a safe, inclusive, and nonjudgmental space to have their questions answered. Despite the challenges, by building relationships with patients and providing factual information, we can create immunity against misinformation.
Image credit: Ivermectin (CC BY-NC 2.0) by focalphoto