Though the white coat’s role in medicine today is complex — to some, a respected symbol of medicine’s history; to others, a antiquated relic of a paternalistic past — few medical students or frontline residents would deny this emblematic item one major utility: a source of pockets.
Dr. Abraham Verghese makes the eloquent case that the objects we keep with us for patient care can serve as important reminders against allowing the “currency” of medical care from centering on the computer rather than the patient.
Perhaps no third-year clerkship leans so heavily on white coat pockets as surgery. At the surgery clerkship at my medical school — as at many others — we students were expected to keep a ready and full stock of supplies. My white coat pockets were generally bulging full.
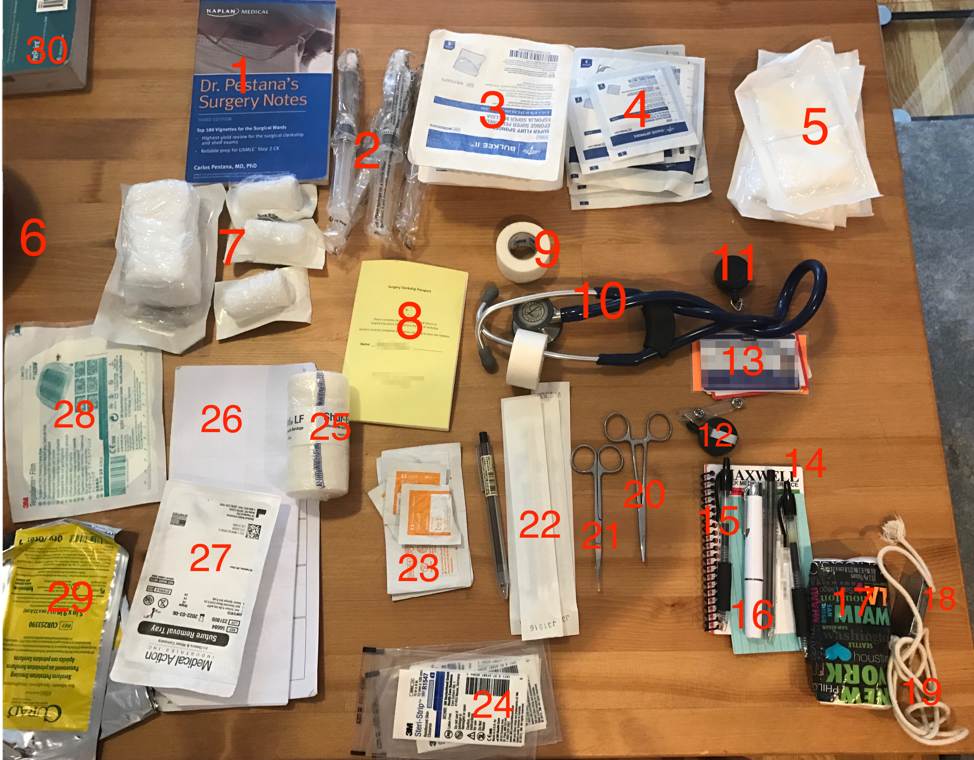
What was in my white coat pockets, Surgery clerkship edition:
- Dr. Pestana’s Surgery Notes: An amazing review book for the surgery shelf exam — both thorough and concise. It’s conveniently-sized to fit into an inner white coat pocket and can also sneak into the back pocket of scrubs for quick reading between cases.
- “Flushes”: 10 mL syringes filled with normal saline, useful for flushing lines or for washing wounds and wetting dressings.
- “Fluffs”: 6 x 6-inch sponges, essential for general wound care. These took up a lot of pocket space, but we went through them by the box-full.
- Square gauze in various sizes: Also used for general wound care and as dressings. We used the “4 by 4s” (4 x 4-inch) most often. I usually had at least two of the larger size.
- ABD pads: Short for “abdominal” and used for larger wounds.
- A shadow
- Gauze rolls: Also used all the time for dressing wounds and holding bandages in place.
- A book with clerkship requirements
- Tape: In two forms: paper and a plastic-like version. The paper is softer on the skin but weaker. Two rolls could easily fit around the tubing of my stethoscope.
- Stethoscope: Used countless times during the day for heart, lung and abdominal auscultation.
- Identification (ID) reel: This was one of the most useful things I bought for third year as it let me extend my ID without unclipping it.
- Extra ID reel: After I had one break during a heavy breeze walking between clinics, I had to use my tie clip to attach my ID to my coat. I’ve since lost that tie clip, but its gallant service has never been forgotten.
- Hospital ID
- Maxwell’s Quick Medical Reference: A great pocket guide with reference material. Even though the electronic medical record and my iPhone made the need for a reference book partly obsolete, it was still incredibly useful being able to look up common values quickly. I often used it to check lab values and remind myself of normal electrocardiogram (EKG) intervals.
- Pens: I spent a lot of time finding the ideal pen for third year — it needed to be clickable for one-hand use and have a fine point for annotating printed documents. I finally settled on two: the Muji 0.38 mm gel-ink ballpoint and the Pilot G2 extra-fine ballpoint. They both served admirably.
- Pocket flashlight: Used just as much for reading pages during the dark hours of early morning rounds as for checking pupils and throats.
- Tissues
- Metal tin with breath mints: Lots of close quarters in surgery especially in the operating room.
- A string: I got this from an old magic trick kit I found at home and used it to practice tying knots. During any downtime between surgeries, my hands could be found tying knots.
- Forceps: These one-time use instruments were for packing wounds, unpacking wounds and for pulling out tight line seals.
- Scissors: For cutting things. Also for one use only.
- Sterile Q-tips: Also good for packing wounds.
- Alcohol prep swabs: For swabbing things.
- Steri-Strips: To close small, mostly-healed or already-sutured wounds.
- Elastic bandage wrap: For tight dressings.
- THE LIST: i.e., The list of patients on the service. Updated every morning, printed, annotated, updated, “run” (reviewed in full) several times a day, updated, re-annotated and always kept within reach. Because I didn’t have space in my pockets for a notebook to jot down teaching points, the back of the list also served a notebook-like purpose.
- Suture removal tray: Appropriately named.
- “Teggies”: Tegaderm, a (mostly) waterproof bandage ideal for sealing gauze, line insertions and more.
- Xeroforms: Lubricated dressings to prevent sticking.
- A corner of Surgical Recall: A great book with details about common surgical procedures for quick review before a case. Only a corner because this 824-page book just happened to be on my table at home and definitely did not reside in my coat pocket.
Strictly speaking, not all of this was in my white coat pockets. Some was obviously attached, such as my ID badge; others were draped around my neck, like my stethoscope; and still more resided in my scrub pockets, such as my cell phone. But, believe it or not, nearly all of this did, with some practice, fit into my white coat. And almost everything pictured got daily use.
Not pictured:
Trauma shears: Only on me while I was on the trauma surgery service.
Snack bar: I relied mostly (by which I literally mean for the majority of my calories) on ProBar Peanut Butter Chocolate Chip meal bars. My daily bar is not pictured likely because I had already eaten it.
iPhone: My phone was essential during third year and was most useful in the hospital for coordinating with my team, looking things up on UpToDate and quick studying.
Card holder: I bought a pouch that stuck to the back of my phone’s case and held all my cards. It was one of the MVPs of third year, allowing me to leave my wallet at home while still keeping my credit card, driver’s license and school ID with me at all times.
Pager: Probably still clipped to my scrubs when I took this picture.