The Forgotten Prescription: Addressing Nutrition Neglect Amongst Medical Students
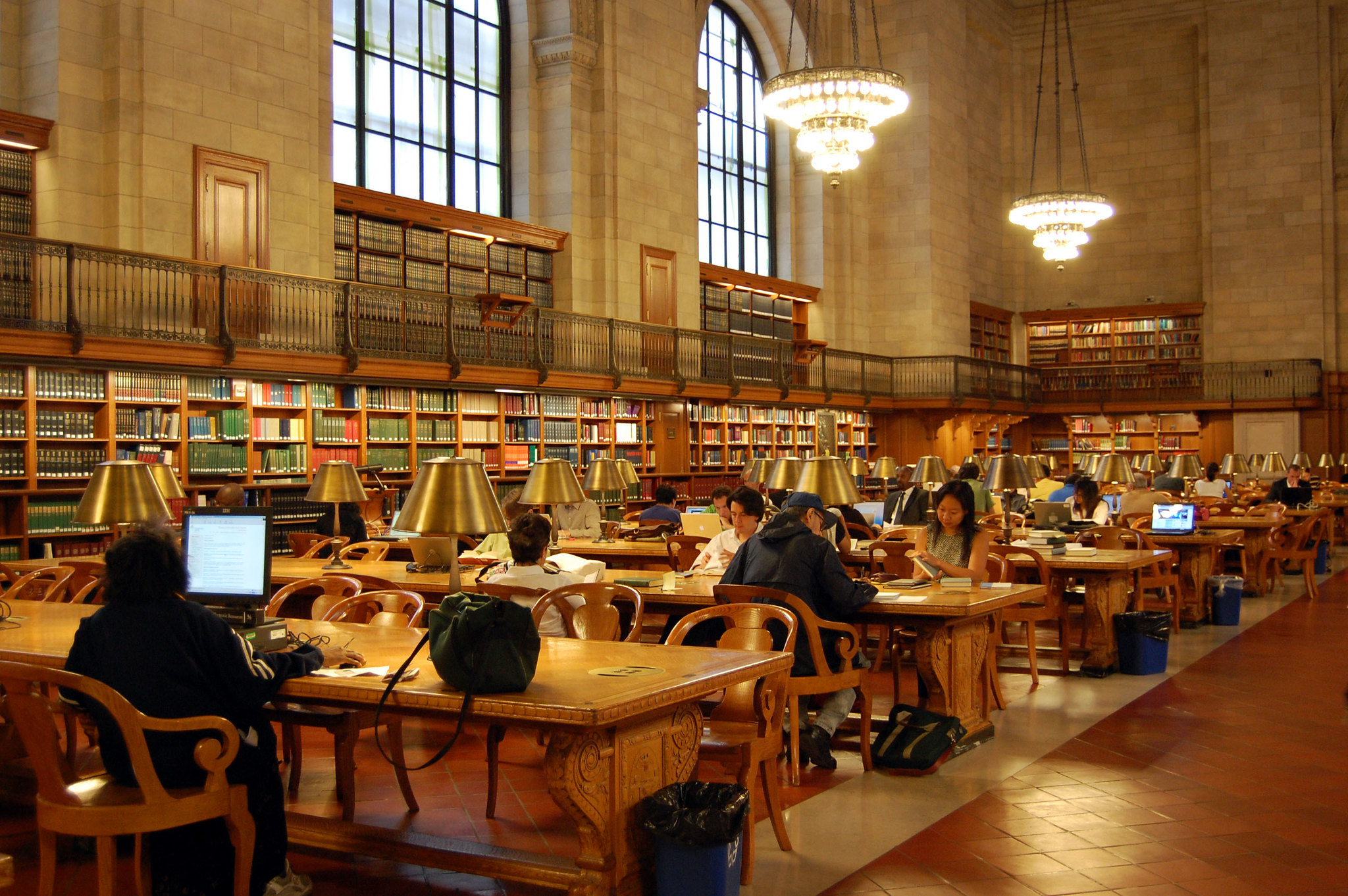
Being a health care professional can, at times, feel ironic because our intention is to promote health and wellness, yet we often neglect our own. As medical students, we consume large amounts of information in short periods of time, which can be both stressful and mentally strenuous. We often must be awake for long hours, whether it’s for rotations, for studying or for both at once. This lifestyle can foster many unhealthy habits, but are …