I should call my mom.
I wish that was the first thought I had after walking out of the patient’s room. Instead, it was, “Damn, that took so long.”
Warm and talkative, she engaged in our conversation in a way that would have been endearing if I wasn’t already stressed out about slowing down the team. After each question I asked, her eyes would light up and she would reciprocate with one of her own. I responded as politely as I could, while keeping my eye on the clock.
She was there for a routine appointment. 64 y/o female with a history of coronary artery disease and a recent cath lab visit.
With her proximal left anterior descending and distal right coronary artery occluded at 74% and 62%, respectively, it appeared that it would soon be time to discuss a coronary artery bypass graft (CABG).
My main job during this visit was to listen to her heart and lungs, ensure that she had done the pre-op labs and imaging and ask the standard medical student list of questions, as well as to answer any basic questions she had.
As I fumbled with the stethoscope and auscultated her heart, it occurred to me that I barely knew what a normal heart sounded like, let alone a crescendo-decrescendo murmur or a diastolic gallop. Stumbling through the interview, I looked up at the clock and noticed I’d already spent half an hour in the room. I quickly wrapped up and presented the case to the attending physician.
I had learned a lot about my patient, though. Maybe too much. She talked about her nephews and their career paths — one was an engineer, the other a scientist. She talked about her excitement to retire and her upcoming trip to Jamaica. I could not shake the feeling that she reminded me of someone I knew.
A week later, I met her in the holding bay bright and early at 6:30 a.m. A few hours later, she was actually in the OR.
Big procedures can be tense, but today’s felt a little different. The atmosphere was relaxed. Jokes were said, my existence was acknowledged and I didn’t even get yelled at by the scrub nurse. The surgery started off really well and it looked like we might even finish early.
Then, unexpectedly, a few issues arose. Two of them, to be precise.
The first: the new anesthesia resident struggled to get the arterial line (which accurately monitors blood pressure) into her radial artery.
The second: the anesthetist let the blood pressure rise too high. In a CABG, when the aorta is penetrated, the pressure should not exceed 75-80mmHg; otherwise, you risk some dangerous complications.
The last few checks involved looking at the heart and aorta with an ultrasound probe to confirm that we were all set. We weren’t. Over the curtain, I heard the dreaded words, “I think I see a dissection?”
Ascending aortic dissection, one of the most feared complications of cardiac surgery. It was expanding and I was politely told to get the hell out of the way. Another surgeon was paged.
A new femoral line was placed. The BP difference between the femoral and radial artery was 30mmHg. As we later found out, we had been over-estimating the BP, because the radial artery line had been incorrectly placed the entire time.
Five more hours of surgery. New aorta. She was now having seizures and the EEG did not look great. Over the weekend, she continued to decompensate.
The patient made it out of surgery alive. Barely. My elective ended that week and I never went back to check on her. I couldn’t stop thinking about her, though, so I looked her name up in the medical record every morning. She died the following Sunday.
I never went back to see the friendly, talkative woman, whose slight hint of an accent came from living in America after growing up in Eastern Africa — the woman who was on the edge of retirement and so excited about it.
I never went back to see her, because almost every detail, down to the way she looked, talked and smiled, reminded me of my mom.
I should call my mom.
Author’s note: All patient modifiers have been modified to protect patient privacy.
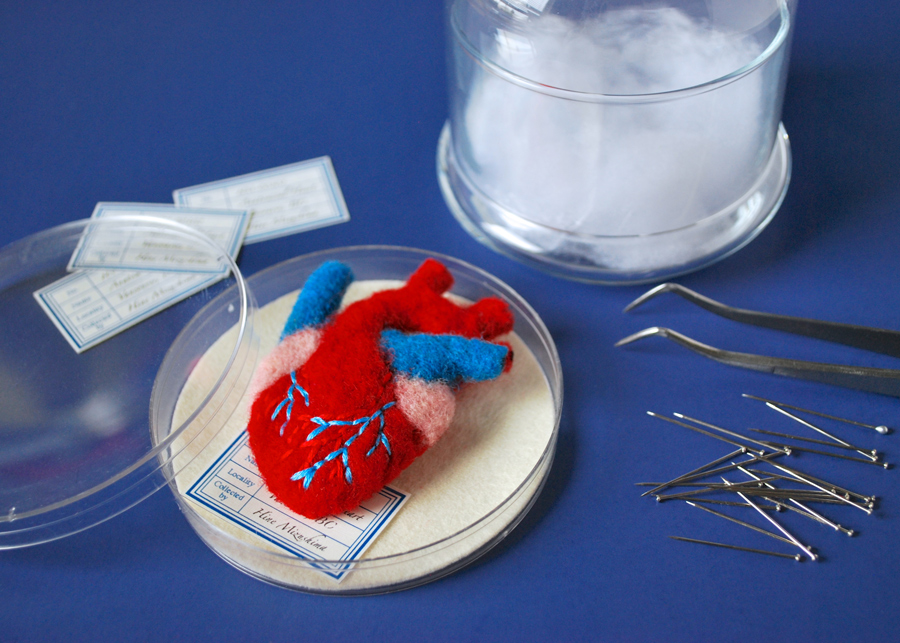
Image credit: Anatomical Heart Brooch (CC BY-NC-ND 2.0) by hine