Ashten Duncan, MPH, CPH (11 Posts)
Ashten Duncan, MPH, CPH (11 Posts)Columnist, Medical Student Editor and Former Managing Editor (2017-2018)
OU-TU School of Community Medicine
Ashten Duncan is a third-year medical student at the OU-TU School of Community Medicine located in Tulsa, Oklahoma. A 2018-2019 Albert Schweitzer Fellow, he recently received his Master of Public Health (MPH) with an interdisciplinary focus from the University of Oklahoma Hudson College of Public Health. Ashten attended the University of Oklahoma for his undergraduate program, completing a Bachelor of Science (BS) in Microbiology and minors in Chemistry and French. An aspiring family physician, Ashten is currently on a National Health Service Corps scholarship. His research interests include hope theory, burnout in medical education, and positive psychology in vulnerable populations. Ashten is passionate about creative writing and what it represents. He has written pieces that have been published on KevinMD.com and in-Training.org and in Blood and Thunder and The Practical Playbook. Ashten is currently serving as Associate Author for the upcoming edition of First Aid for the USMLE Step 1.
The Lived Experience
As medical students, we sometimes lose sight of our purpose for going into medicine and feel that we are exerting ourselves excessively with little feedback from our environment. It is important that we remember that, while we are living through the experiences that come with our training, our future patients are also living through their own experiences. The focus of this column is to examine topics in positive psychology, lifestyle medicine, public health and other areas and reflect on how these topics relate to medical students, physicians and patients alike.
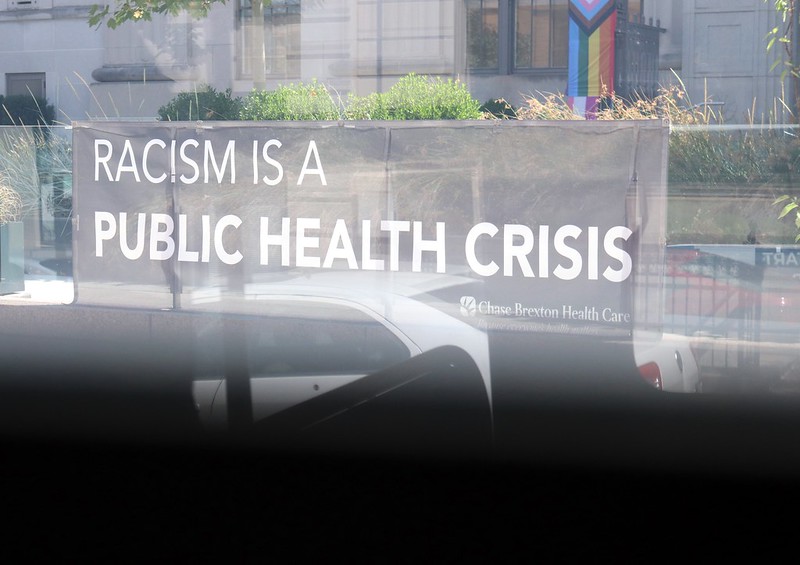
Current evidence suggests that much of human health is influenced more significantly by contextual factors like the social determinants of health than the direct receipt of health care. This relatively new understanding has challenged the notion of “physicianhood” and what it means to improve the health of entire populations and communities. With the influx of issues that the pandemic has brought with it, this new model for being a highly effective physician has become even more important.
We will recall when, during the summer of 2020, the moral and political duty to engage with the most momentous anti-racist movement since the 1960s reanimated a nation paralyzed by fear. By the fall, cataclysmic wildfires on the West Coast poisoned the air from San Francisco to New York City. Coronavirus, cultural upheaval and manifestations of climate change all bore down on us as we entered the most consequential and divisive national election in living memory.
Mercedes drove two hours to the nearest healthcare clinic to get her first physical exam in ten years. I met Mercedes while shadowing a primary care physician, Dr. L. In the clinic, Mercedes divulged to me how nervous she had been driving in – she knew what the meeting held in store. Her fears were confirmed: just five minutes into her exam, Dr. L advised her, “Mercedes, you have to lose weight.”
Moreover, homelessness and COVID-19 both disproportionately burden marginalized populations — in particular, Black communities and Native Americans. When COVID-19 began spreading through the community, it came as no surprise that it would disproportionately impact those living in congregate homeless shelters. Overcrowded shelters, the inability to physically distance, and poor access to handwashing and hygiene facilities are coalescing for an unsafe environment that could accelerate disease transmission.
As stressed medical students looking for an eventful destination to spend our spring break, my friend and I chose to take a trip to America’s Big Apple, New York City. On a sunny day in NYC, I remember enjoying our morning cups of coffee and walking into a subway station when, suddenly, an older man shouted at us, “Take your corona and get out of my country!”
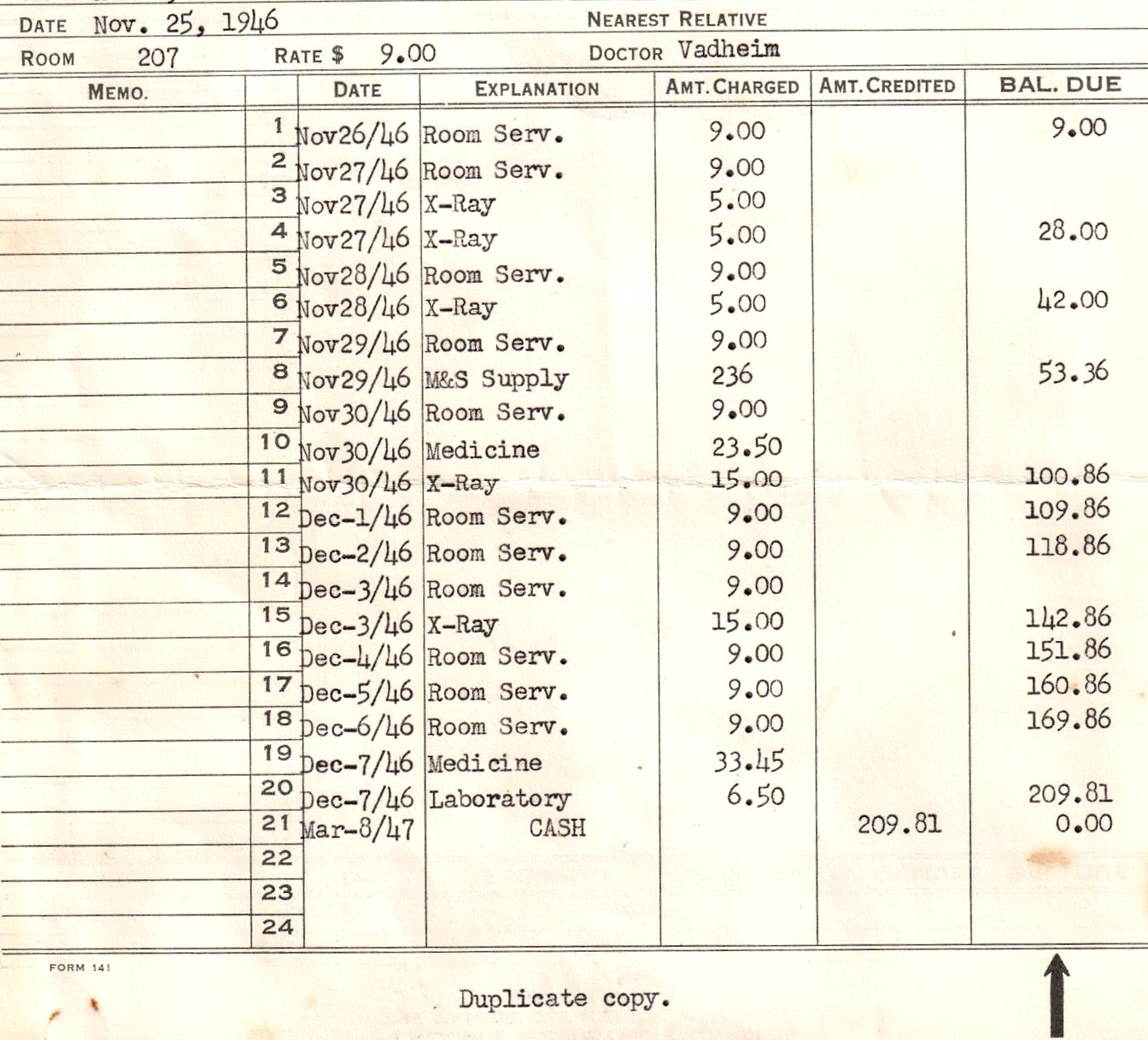
There is a cost crisis in medicine: the health care industry accounts for about 18 percent of the GDP in the United States, and predictive models see this increasing in the coming years. This is a problem for the country as a whole as an estimated 41 percent of working Americans have some level of medical debt.
I have learned that patients seek health care services at free clinics for a myriad of reasons and some are atypical. There were specific populations I expected to see: the uninsured, underinsured, undocumented, and those without access to transportation. Yet there were other populations I was more surprised to see, namely patients who had insurance but preferred their experiences at free clinics.
President Trump signed an executive order this past June that directs the Health and Human Services Department to develop a rule requiring hospitals to disclose online the prices that insurers and patients pay for common items and services. The rule also requires hospitals to reveal the amounts they are willing to accept in cash for an item or service. However, hospitals not complying only face a civil penalty of $300 a day, giving them latitude to effectively ignore the executive order.
“Defund the police” has become one of the slogans of the protests shaking our nation amidst the COVID-19 pandemic. But what does this term truly mean, and could defunding the police be helpful for both the police and the health care community?
Hahnemann’s doors stay closed and our patients are waiting. While Philadelphia has stopped negotiations, we, as students with futures in health care, cannot accept this. We demand that Freedman provide free use of Hahnemann for the duration of the pandemic.
Throughout my training, I’ve observed the shortcomings and strengths of the health care system from the perspective of the next generation of physicians. Lack of emphasis on preventative care put Americans at risk even before COVID-19 hit our shores.
From a public health perspective, we in Oregon have nowhere near the number of cases as our northern neighbors in Washington, although with delayed testing it is hard to tell exactly how many people are infected. But as we continue to follow the pattern of disease spread that has been demonstrated in Wuhan and Italy, we can presume that things will only escalate from here. And with it, inequities will be laid bare.
 Brett Lewis (1 Posts)
Brett Lewis (1 Posts)Contributing Writer
Oregon Health & Science University
Brett Lewis is a third year medical student at Oregon Health & Science University in Portland Oregon class of 2021. In 2014, she graduated from UC Berkeley with a Bachelor of Arts in public health with a minor in anthropology. After medical school, she worked as Program Coordinator of the UCSF HEAL Initiative, an organization that trains fellows from or who are dedicated to serving communities in Navajo Nation and countries such as Liberia, Haiti, and Mexico. She enjoys reading, running, and racing cyclocross in her free time. After graduating medical school, Brett would like to pursue a combined career in family medicine and psychiatry.