One of the most impactful influences on my decision to become a doctor was meeting a patient with multiple sclerosis (MS). I was 19 years old and a hospital volunteer in Michigan. As I was replacing gloves, gowns and towels in my department, I entered the room of an elderly Eastern-European woman. After a brief introduction, I noticed that she had many peculiar traits. Not only did she appear extremely fatigued, but her limbs were stiff when she moved, she frequently needed to use the bathroom and even speaking appeared difficult.
After some efforts mumbling and muttering, she excused herself and clarified that she had relapsing-remitting multiple sclerosis. Being curious and not knowing a lot about MS, I asked her what the disease was and what it was like for her to have it. Her story remains with me to this day. She had been a piano player in her twenties with a “God-given talent” for jazz. It wasn’t until she was almost thirty that things began to feel “off”: formerly routine jogs suddenly became difficult, her back began to have tremendous pain, and worst of all, she started hitting the wrong keys as she played the piano.
When she and her mother received news from a neurologist that she did indeed have multiple sclerosis, her mother started crying. Being a social worker, her mother was aware of the hardships that people with multiple sclerosis face in performing even basic activities of daily living — not to mention the haunting fact that there is no cure. However, after initially being diagnosed, medications and physical therapy did improve her symptoms considerably. Well… until this recent hospital visit, when her symptoms relapsed.
Fascinated, yet dismayed by her story, I asked her what the toughest part about having MS was. With no hesitation she said, “Losing my independence.” The conversation came to a halt when her mother arrived in the room and asked to have some privacy to talk to her. I obliged, finished cleaning up the countertops and left the room as they began to chat. As I closed the door, I glanced back to see her mother hoisting her from the bed so she could use the bathroom — a scene I will never forget.
A few years later, I found out that one of my distant relatives was also diagnosed with multiple sclerosis. According to his wife, he had all the classic symptoms that came with it — fatigue, muscle weakness, urinary incontinence and more. It was a curious phenomenon to me that an Eastern European woman and an Indian man would both have the exact same illness with no known close family history of the disease. Both my relative and the woman I met in college revealed to me how incapacitating and nondiscriminatory MS can be. While this horrible disease has demonstrated a slight preference for particular genders, races and ethnicities, the reality is that MS itself can affect anyone at almost any time.
Entering medical school, I hoped that I would glean more answers to my questions — how do diseases like MS impact the body? What treatments are there for MS and how much research and advocacy work is being done for those diagnosed? Sadly, MS was addressed in a few neuroanatomy and immunology lectures during my first year of medical school. It was useful as an introduction and overview on the topic, but it left me craving more real-world knowledge on what to do to treat it. With that, I was all the more ecstatic to be accepted into the 2021 Virtual Clinical Mentorship Program as part of the National Multiple Sclerosis Society (NMSS).
I had initial reservations about how well a virtual program could dive deep into MS. How would we even see patients with so many COVID restrictions in place? Fortunately, the two-week program proved unexpectedly rewarding. Most of my time was encompassed by specific, informative and practical didactic lectures. In contrast to my first-year courses, these didactics had sufficient time to address MS with the depth it deserves. In particular, Dr. Suma Shah’s lecture, “MS Across the Lifespan,” which described the diverse phenotypic expressions of MS, and how it can be influenced by genetics, age, sex and environmental factors, was particularly memorable and relevant to me as a future clinician. Along with the lectures, we had a “Patient Experience” session where my cohort and I had the opportunity to ask patients with MS about their personal stories and how they’ve changed since receiving the diagnosis. Moreover, I learned about “MS Navigators,” medical professionals and volunteers who help newly-diagnosed MS patients find a sense of community, a vital part of recovery and alleviation of symptoms.
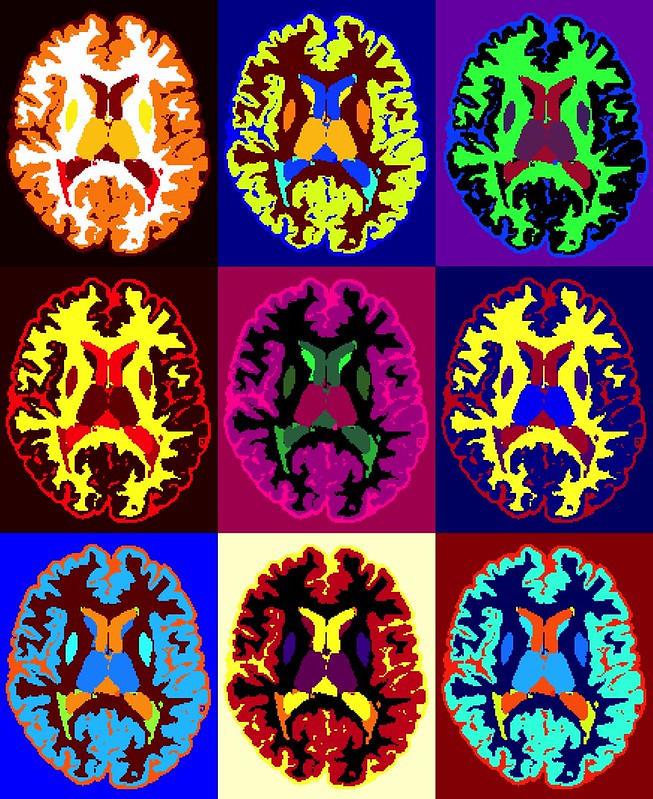
In addition to the didactics, I had the opportunity to observe Dr. Francesca Bagnato’s practice and research at the MS Clinic at Vanderbilt University. After touring her lab and learning about her research, which primarily involves neuroimaging of periventricular lesions, I spent the rest of the day shadowing her teleneurology appointments. I admired the way she was able to integrate her scientific research into her practice and vice versa; it helped remind me of my own passion to do the same as a future physician. After shadowing Dr. Bagnato and completing the whole mentorship program, I was inspired by the variety in clinical practice, research, advocacy work and more that one can achieve as a neurologist. The NMSS’s Virtual Clinical Mentorship Program made it clear that there are many career opportunities and pathways for future neurologists who desire to specialize in MS in their future practice.
When the program ended, I imagined that it would mark the end of my tryst with learning about multiple sclerosis for a while. I wondered if all the knowledge and interest I had developed would fade into another distant memory or line on my residency application. I assumed that I wouldn’t see it again until my rotations began, at best. As it turned out, however, I would encounter this condition again in my personal life, just weeks later.
In the remaining weeks of that same summer, I put my initial busyness with the program behind me and took a solo trip to Portland, Maine for some relaxation. During a chance visit to a local laundromat, I started a dialogue with the laundromat owner. One topic led to another, and unexpectedly, she disclosed her own diagnosis of relapsing-remitting multiple sclerosis.
Immediately, I noticed how much better I could relate to her experience with MS as compared to my past encounters with the patient I met or even with my relative: I internally considered her risk factors (being a woman of Northern European descent, probably in her twenties), understood why her symptoms would be worse in the winters of Maine than in the summer, and most personally, I could understand how the fatigue was an absolute nightmare, inhibiting her ability to work and support her family. Furthermore, unlike during my prior encounters, I could now ask intelligible questions about her physical therapy program and immunosuppressive medication regimen. I could now remember more about possible side effects that she may have experienced and ask her about the presence of other autoimmune disorders. And better yet, I could now instill some more meaningful, kind words regarding her own strength — especially her ability to operate a small business despite the drastic, chronic condition with which she battles every day.
As our conversation came to a close, I found myself feeling… fuller. Fuller with the satisfaction of applying my recently-obtained knowledge to a real life situation. Fuller with the sense of progress, seeing myself relate to patients suffering from a unique illness about which I had such little understanding so recently. And fuller with the anticipation of repeating this process of learning and application time and again in my future career. It is, indeed, relapsing and remitting — only unlike MS, it’s better for it to stay.
Image credit: Axial MRI scans of a person (Public Domain) by National Institutes of Health (NIH)