Taking a Wider View: A Medical Student’s Perspective on Reforming Obesity Medicine Training
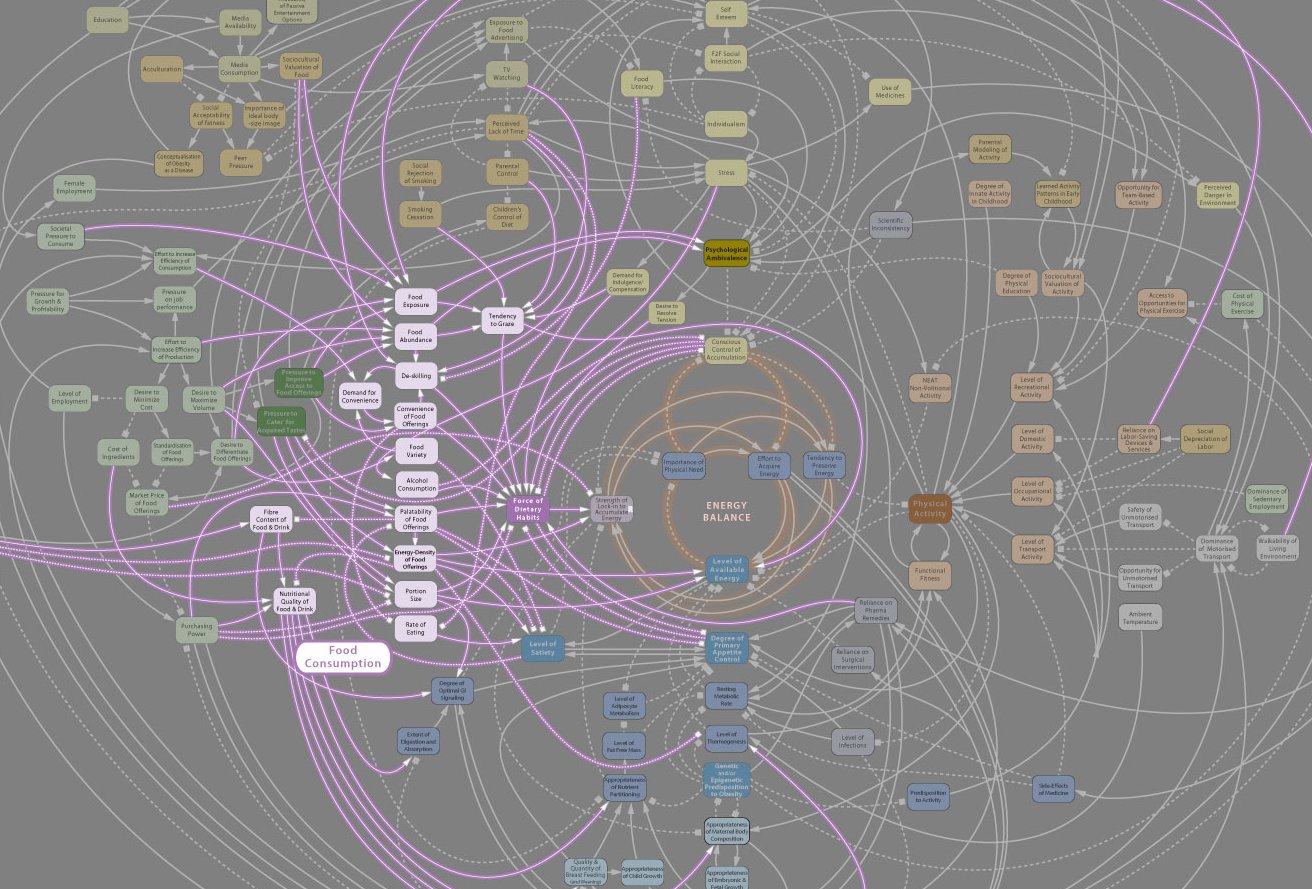
As physicians, we must work to lift patients up when they are struggling, rather than shaming them into well-being. As Dr. Donald Berwick once noted, it is not always patients’ diagnoses, but their helplessness that kills them. Indeed, the helplessness we instill through our focus on individualism and molecular pathology in the clinical setting will ensure that this epidemic kills millions prematurely and costs billions of dollars. If obesity is a disease caused by society — its inequities, trauma, and expectations — then the solution for obesity should address more than just the patient sitting in front of us.